 The 14 hospital trusts to be looked at as part of a rapid, independent, national investigation into maternity and neonatal services were named on 15 September 2025 by the Department of Health and Social Care (DHSC).
The 14 hospital trusts to be looked at as part of a rapid, independent, national investigation into maternity and neonatal services were named on 15 September 2025 by the Department of Health and Social Care (DHSC).
Baroness Valerie Amos’s investigation will put families at the heart of the work, the DHSC said, and affected families were asked to provide input to the draft terms of reference of the investigation. The terms of reference have been developed to focus on understanding the experiences of affected women and families, identifying lessons learned and driving the improvements needed to ensure high-quality and safe maternity and neonatal care across England.



 By Tonia Goman of Skin Camouflage Bristol
By Tonia Goman of Skin Camouflage Bristol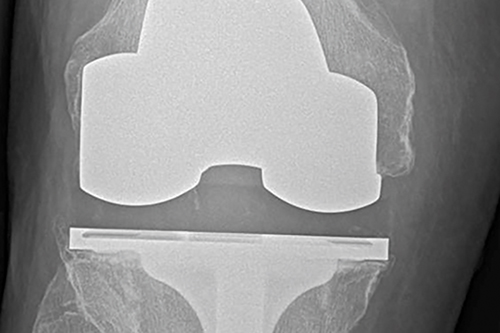 Researchers from the Musculoskeletal Research Unit at the University of Bristol have found that eight out of 10 total knee replacements and six out of 10 total hip replacements will still be in place after 25 years. The research, funded by the National Joint Registry and the National Institute for Health Research was published in The Lancet in February.
Researchers from the Musculoskeletal Research Unit at the University of Bristol have found that eight out of 10 total knee replacements and six out of 10 total hip replacements will still be in place after 25 years. The research, funded by the National Joint Registry and the National Institute for Health Research was published in The Lancet in February. In September the Ministry of Justice published the results of a consultation on medical reporting within the package of whiplash and small claims track reforms – due to be implemented in April next year for road traffic cases. The consultation ran for a month in April-May, and the resultant document sets out the government’s policy choices.
In September the Ministry of Justice published the results of a consultation on medical reporting within the package of whiplash and small claims track reforms – due to be implemented in April next year for road traffic cases. The consultation ran for a month in April-May, and the resultant document sets out the government’s policy choices. Doctors are increasingly expected to provide patient care in unsafe environments, where a persistent culture of blame stifles learning and discourages innovation. That is the conclusion drawn from a BMA survey: part of an ambitious project aiming to find solutions to the challenges faced by the NHS.
Doctors are increasingly expected to provide patient care in unsafe environments, where a persistent culture of blame stifles learning and discourages innovation. That is the conclusion drawn from a BMA survey: part of an ambitious project aiming to find solutions to the challenges faced by the NHS.